Heart failure, sometimes called congestive heart failure, is a chronic condition where the heart muscle is unable to pump enough blood to meet the body’s needs. It doesn’t mean the heart has stopped working, but rather that it’s working less efficiently. Individuals at risk include older adults, those with a history of heart disease, high blood pressure, or diabetes. Early diagnosis and treatment are essential to improve quality of life and prevent further deterioration of heart function.
Causes & Risk Factors
Heart failure can result from various underlying conditions that damage or weaken the heart muscle. Common causes include coronary artery disease, previous heart attacks, high blood pressure, heart valve disease, and cardiomyopathy. Genetic factors can also play a role. Major risk factors that contribute include smoking, obesity, diabetes, high cholesterol, and sleep apnoea. These factors strain the heart over time, leading to heart failure.
Symptoms
Symptoms of heart failure can vary depending on the severity and type. Common signs include shortness of breath (especially during exertion or at night), fatigue, swelling in the legs and ankles (oedema), rapid or irregular heartbeat, and persistent coughing or wheezing with white or pink blood-tinged mucus. Mild heart failure might cause symptoms only during strenuous activity, while severe heart failure can cause symptoms even at rest. If you experience sudden shortness of breath, chest pain, or fainting, seek immediate medical attention.
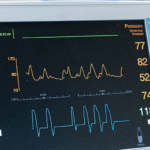
Diagnosis
Diagnosing heart failure involves a combination of medical history, physical examination, and diagnostic tests. An echocardiogram is the primary imaging test to assess the heart’s structure and function. Blood tests can check for markers of heart failure, such as BNP (B-type natriuretic peptide). An electrocardiogram (ECG) can detect abnormalities in heart rhythm. Chest X-rays can show enlargement of the heart or fluid buildup in the lungs. Early detection allows for timely intervention and management.
Treatment Options
Treatment for heart failure aims to manage symptoms, slow disease progression, and improve quality of life. Lifestyle changes are crucial, including a low-sodium diet, fluid restriction, regular exercise (as tolerated), and smoking cessation. Medications like ACE inhibitors, beta-blockers, diuretics, and digoxin can help improve heart function and relieve symptoms. In some cases, medical procedures such as pacemaker or defibrillator implantation, or heart transplantation may be necessary.
Complications & Risks
Untreated heart failure can lead to serious complications, including kidney damage, liver damage, and pulmonary hypertension. The reduced blood flow can affect various organs. Chronic heart failure can significantly impact quality of life, causing fatigue, shortness of breath, and limiting daily activities. Hospitalisations are common for acute exacerbations.
Prevention & Management
Preventing heart failure involves managing underlying conditions and adopting a heart-healthy lifestyle. This includes controlling blood pressure, cholesterol, and diabetes, maintaining a healthy weight, eating a balanced diet, exercising regularly, and avoiding smoking and excessive alcohol consumption. Regular check-ups with your doctor are crucial for monitoring heart health and detecting any changes. Managing existing heart conditions is essential to prevent progression to heart failure.
If you’re experiencing symptoms of heart failure or have concerns about your heart health, it’s important to seek medical advice. Our experienced cardiologists can provide comprehensive evaluations, accurate diagnoses, and personalised treatment plans to help you manage your heart failure and improve your quality of life. Don’t let heart failure limit your life. Schedule a consultation today and take control of your cardiac health.