Cardiomyopathy is a disease of the heart muscle, making it harder for the heart to pump blood effectively. There are several types, including dilated, hypertrophic, and restrictive cardiomyopathy. Anyone can develop cardiomyopathy, but certain factors increase risk, such as a family history of the condition, high blood pressure, or past heart attacks. Early diagnosis and treatment are crucial to manage symptoms and prevent heart failure.
Causes & Risk Factors
Cardiomyopathy can have various causes. Genetic mutations are a significant factor, especially in hypertrophic cardiomyopathy. Other causes include viral infections, long-term high blood pressure, alcohol abuse, drug use, and certain medical conditions like diabetes or thyroid disorders. Major risk factors that contribute include obesity, smoking, and a sedentary lifestyle. In some cases, the cause remains unknown (idiopathic).
Symptoms
Symptoms of cardiomyopathy can vary depending on the type and severity. Some people may experience no symptoms in the early stages, while others may develop shortness of breath, fatigue, swelling in the legs and ankles, chest pain, or palpitations. Mild cardiomyopathy might cause occasional discomfort, while severe cardiomyopathy can lead to heart failure. If you experience persistent shortness of breath, chest pain, or fainting, seek immediate medical attention.
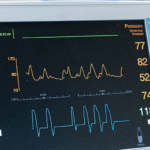
Diagnosis
Diagnosing cardiomyopathy involves a combination of medical history, physical examination, and diagnostic tests. An echocardiogram is the primary imaging test to assess the structure and function of the heart muscle. An electrocardiogram (ECG) can detect abnormalities in heart rhythm. Blood tests can check for markers of heart failure or other underlying conditions. Cardiac MRI or coronary angiography may be used for further evaluation. Early detection is vital for effective management and to prevent complications.
Treatment Options
Treatment for cardiomyopathy aims to manage symptoms, slow disease progression, and prevent complications. Lifestyle changes are often recommended, including a heart-healthy diet, regular exercise, and smoking cessation. Medications like ACE inhibitors, beta-blockers, diuretics, and anticoagulants can help control symptoms and improve heart function. In some cases, medical procedures like pacemaker or defibrillator implantation, septal ablation, or heart transplantation may be necessary.
Complications & Risks
Untreated cardiomyopathy can lead to serious complications, including heart failure, arrhythmias, and sudden cardiac arrest. The weakened heart muscle can struggle to pump enough blood, leading to fluid buildup and organ damage. Chronic cardiomyopathy can significantly impact quality of life, causing fatigue, shortness of breath, and limiting physical activity.
Prevention & Management
Preventing cardiomyopathy involves adopting a heart-healthy lifestyle. This includes maintaining a healthy weight, eating a balanced diet, exercising regularly, and avoiding smoking and excessive alcohol consumption. Regular check-ups with your doctor are crucial for monitoring heart health and detecting any changes. Managing underlying conditions like high blood pressure or diabetes is also essential.
If you’re experiencing symptoms of cardiomyopathy or have concerns about your heart health, it’s important to seek medical advice. Our experienced cardiologists can provide comprehensive evaluations, accurate diagnoses, and personalised treatment plans to help you manage your cardiomyopathy and improve your quality of life. Don’t let heart muscle disease limit your life. Schedule a consultation today and take control of your heart health.